Aetna for Therapy
Aetna is one of the largest health insurance companies in the U.S., with coverage that includes mental health, behavioral health, and therapy services. This guide outlines the coverage that Aetna typically provides for therapy services.

Does Aetna Behavioral Health cover therapy?
Yes, nearly all Aetna Behavioral Health plans cover therapy for mental and behavioral health conditions.
Health insurances offered through the health insurance Marketplace or through small employers are required by the Affordable Care Act to cover mental health services. While not required by federal law, the vast majority of large employers also cover mental health services.
While rare, your Aetna plan may not cover therapy services if:
- You work for a large employer that does not include mental health benefits in its insurance coverage.
- Your health insurance plan was created before 2014, when the ACA’s requirement that health insurance plans cover mental health services was enacted.There are other situations in which your Aetna plan may not cover the specific type of therapy service you are seeking, or where your coverage may not apply until you spend a certain amount on medical services first. Learn more about these cases below.
How do I check if my Aetna plan covers therapy?
To check whether your Aetna plan covers therapy, look for the “Outpatient Mental Health” line item on your Summary of Benefits.
Therapy is considered a type of outpatient mental health service. You can find your Summary of Benefits by logging into your Aetna Member Services portal (called “myAetna”), calling member services, or checking your employer’s benefits portal.
Here is an example of what your Aetna Summary of Benefits may look like, and where to find the Outpatient Mental Health line item:
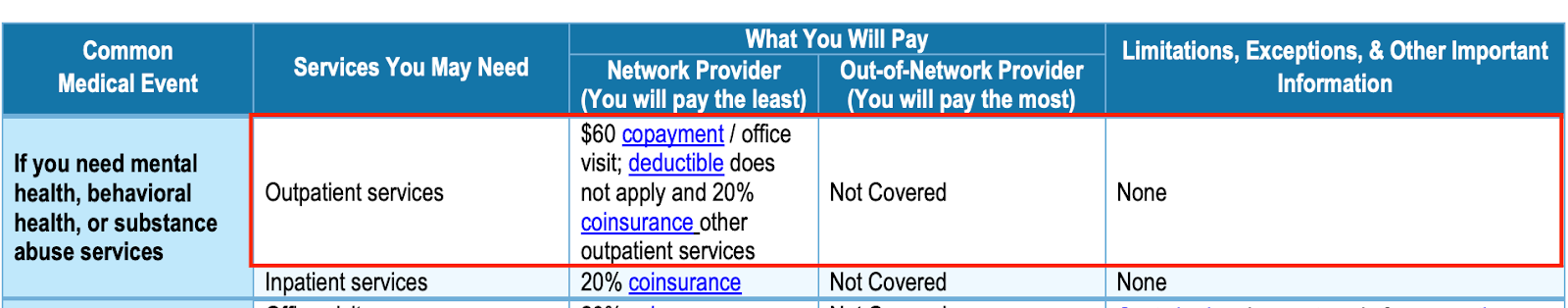
If the Outpatient Mental Health line item indicates that these services are not covered, then your health insurance plan does not cover therapy services.
If you cannot find coverage information for Outpatient Mental Health, you can contact Aetna for assistance. If you receive health insurance through your employer, reach out to your employer’s human resources department.
While your Aetna plan likely covers therapy, the extent of coverage and requirements for coverage depend on your particular plan. Read on to learn more.
How much does therapy cost with an Aetna Behavioral Health plan?
The cost of therapy sessions with Aetna depends on your plan’s coverage: in the best case scenario, your therapy sessions may be fully covered, meaning you don’t pay anything at the time of session; most likely, the cost ranges from $15 to $50 per session. In the worst case scenario, you need to pay the full fee that the therapist charges at the time of the session, which generally ranges from $80 - $200 per session. Find the scenario that applies to you below:
If you choose a therapist who is in-network with Aetna, your therapy sessions likely cost between $15 - $50 per session, after you meet your deductible. The $15 - $50 amount is your copay, or the fixed amount that you owe at each therapy visit. The deductible is the total amount you need to spend in medical costs in any given year before your health insurance begins to cover the cost of services. Here are examples you may see on your Summary of Benefits under the “In-network Outpatient Mental Health” category and what they mean:
- $15 copay, after $5,000 deductible → After you spend $5,000 in medical costs this year, your therapy sessions will cost $15 per session.
- $15 copay, after $1,000 deductible → After you spend $1,000 in medical costs this year, your therapy sessions will cost $15 per session.
- $15 copay, deductible does not apply → Your therapy sessions will cost $15 per session regardless of your deductible amount (ie. even if this is your first medical visit of the year, you will only pay $15 at the time of your therapy session).
If you choose a therapist who is not in-network with Aetna and you have a Aetna PPO Plan, your therapy session will likely cost between $50 - $100 per session, or 20% - 50% of the full amount that your therapist charges per session. This percentage is called a coinsurance: you pay the therapist’s full fee at the time of the session, send a claim to your health insurance company, and receive a check or direct deposit for the remaining percentage that your plan covers. PPO plans typically only cover out-of-network services after you meet your deductible. Here are examples you may see on your Summary of Benefits under the “Out-of-Network Outpatient Mental Health” category and what they mean:
- 20% coinsurance, after $5,000 deductible, therapist charges $100/session → After you spend $5,000 in medical costs this year, your plan will reimburse you $80 of your therapy session fee; your effective therapy cost is $20/session.
- 20% coinsurance, after $1,000 deductible, therapist charges $150/session → After you spend $1,000 in medical costs this year, your plan will reimburse you $120 of your therapy fee each time you submit a claim; your effective therapy cost is $24/session.
If you choose a therapist who is not in-network with Aetna and you have a Aetna HMO or EPO Plan, your plan will likely not reimburse you for sessions with a therapist who is not in-network with Aetna. You would owe the therapist’s full fee at the time of session and not receive reimbursement from your plan. If cost is a barrier to seeking therapy, you can look for a therapist who offers a sliding scale, or lower session fees based on financial need.
What types of therapy does Aetna cover?
The modalities that Aetna Behavioral Health covers may include, but are not limited to, the following:
Any therapy type that is evidence-based and utilized for the purposes of diagnosis and treatment of mental health conditions should be covered by Aetna plans.
What kinds of therapy does Aetna not cover?
Like most insurances, it is not typical for Aetna to cover services unrelated to a diagnosable mental health condition, such as:
- Couples counseling - Couples counseling is typically not covered by insurance, because relationship issues, while a significant source of stress, are not considered a diagnosable mental health condition.
- Life coaching - Life coaching is not covered by insurance because it focuses on achieving personal goals, rather than treating a diagnosable mental health condition.
- Career coaching - Career coaching is not covered by insurance because it focuses on achieving professional goals, rather than treating a diagnosable mental health condition.
Aetna is also unlikely to cover therapy sessions occurring outside the therapy office, because of the greater potential for risk involved.
While clients may sometimes benefit from services rendered outside of the therapy office, such as a client with an eating disorder needing support in the grocery store, or a client with a phobia of driving needing support in the car, these services are not likely to be covered by insurance and must be paid for out-of-pocket.
Does Aetna Behavioral Health cover couples therapy?
No. While it depends on your specific plan, it is unlikely that Aetna will cover couples counseling.
That said, even if your insurance doesn't directly cover it, you still have options for getting affordable couples counseling. Here are five ways to pay for couples counseling if it’s not included in your health insurance plan.
Do I need to see my doctor before visiting an Aetna therapist?
If you need to see your primary care doctor before visiting a Aetna therapist depends on your insurance plan type:
- HMO or POS plan: Yes, you are typically required to see your primary care physician for a referral to therapy before Aetna will pay for services
- PPO or EPO plan: No, you typically don’t need to see your primary care physician for a referral to therapy before Aetna will pay for services.
This referral requirement is also called pre-authorization (or prior authorization). Pre-authorization is a process where a health provider, in this case your therapist, must get approval from your insurance company before providing you with care in order for the services to be covered.
Your Summary of Benefits should indicate whether you need pre-authorization for outpatient mental health services.
Does Aetna Behavioral Health cover online therapy?
Yes, Aetna does usually cover video therapy sessions, which you can use in place of an in-person visit to your therapist’s office.
Video sessions are also an option for managing medications without an office visit.
Find vetted therapists who are in-network with Aetna
- Alabama
- Alaska
- Arizona
- Arkansas
- California
- Colorado
- Connecticut
- Delaware
- Florida
- Georgia
- Hawaii
- Idaho
- Illinois
- Indiana
- Iowa
- Kansas
- Kentucky
- Louisiana
- Maine
- Maryland
- Massachusetts
- Michigan
- Minnesota
- Mississippi
- Missouri
- Montana
- Nebraska
- Nevada
- New Hampshire
- New Jersey
- New Mexico
- New York
- North Carolina
- North Dakota
- Northern Mariana Islands
- Ohio
- Oklahoma
- Oregon
- Pennsylvania
- Puerto Rico
- Rhode Island
- South Carolina
- South Dakota
- Tennessee
- Texas
- Utah
- Vermont
- Virginia
- Washington
- Washington DC
- West Virginia
- Wisconsin
- Wyoming